Respiratory Health: How to Build A Resilient Lung Microbiome

On a recent trip to Ghana, I was exposed to a combination of pollution and Harmattan dust winds which exacerbated my asthma. While it is evident that the air quality driving along long dusty roads was hurting my lungs, I was curious if the stress of travel and an upset digestive system could contribute to my respiratory problems.
Mucosal surfaces in the lungs are exposed to the external environment and are highly susceptible to pollution and bacterial and viral infections. But research shows that lung health is also be influenced from within. It appears that the gut and even our state of mind impact lung health through a pathway that links the brain, gut, and lungs called the gut-brain-lung axis.
Immunity and the Lung Microbiome
From the moment we take our first breath, our microbiome starts to take shape, influenced throughout life by the food we eat, the air we breathe, and the environment we live in. These trillions of microorganisms – bacteria, viruses, and fungi – interact with our immune system in the gut, skin, and lungs.
Our immune system continuously processes the information our microbiomes translate from environmental stimuli. Living in an urban environment brings challenges that require us to take extra measures to support our health, including our lungs, so our immune system keeps us well protected.
How does stress influence lung health?
Stress weakens lung immunity. A research paper published in Thorax 2006 showed that negative emotions such as anger, sadness, and anxiety increased pro-inflammatory messengers triggering asthma and increased susceptibility to viral infections.
In athletes respiratory problems are a common occurrence where lung immunity is compromised by increased training loads, travels and sleep disruptions.
How does pollution affect the lungs?
According to the World Health Organization (WHO), nine-tenths of the world's population breathes polluted air, which claims the lives of 7 million people every year globally. Poor air quality causes lung inflammation and scarring. Cigarette smoke is the leading cause of Chronic Obstructive Pulmonary Disease, and mycotoxins from fungal spores affect people living in damp buildings.
Airborne particulate matter such as asbestos, silica, heavy metals from paint, and additional sources of indoor air pollution also contribute to respiratory disease.
Recurrent bronchitis episodes not responding to antibiotics or even the best herbal therapies may require a careful evaluation of the air quality in our homes and workplace.
Keep a clean home, wash linens, vacuum, dust, and replace air filters regularly. Consider wearing a mask in polluted areas, traveling, and crowded places.
Does weight gain affect lung health ?
The connections between obesity and lung problems may not seem so obvious at first. The accumulation of fatty tissue in our body contributes to a low-grade state of systemic inflammation. Obesity enhances pulmonary inflammation triggered by environmental exposures and exacerbates airway obstruction.
Does metabolic syndrome affect my lungs?
Metabolic syndrome is initially characterized by insulin resistance, abdominal obesity, hypertension, and hyperlipidemia. But people with average weight can have metabolic syndrome too.
Research shows that an increased fat to muscle mass ratio is the actual cause of metabolic syndrome promoting inflammation and insulin resistance.
For the lungs, increased systemic inflammation elevates vulnerability to viral and bacteria, increasing the risk for asthma, chronic obstructive pulmonary disease, and lung cancer.(4,5,6)
How does the gut affect lung health ?
Microbes that reside in the gut produce enzymes that convert food into metabolites and impact immune function when absorbed into the bloodstream. The gut and the lungs are connected through a complex web of immune messengers called the typical mucosal response.
Gut microbiome imbalances has been implicated in asthma, chronic obstructive pulmonary disease (COPD), cystic fibrosis (CF), lung cancer, and respiratory infection. Living in an urban setting reduces gut microbiome diversity increasing the lungs' vulnerability to these conditions.
Also, the recurrent use of antibiotics affects the gut and increases susceptibility to the influenza virus; vice versa, lung changes can change gut function. On the other hand research also shows that lungs infected by influenza can trigger imbalances in the gut microbiome.(8)
How can I improve my lung health?
William Cookson, Professor of Genomic Medicine at Imperial College London, shared in an interview with Newsweek that dietary changes could modify the severity of viral infections such as COVID-19.
In the same article, Glenn Gibson, professor of Food Microbiology at the University of Reading, stated, "The gut microbiome is critical to health and well-being, impacting upon a variety of important disorders." Gibson says he has been advising people to take prebiotics and probiotics that boost gut microbial health "for weeks" during the Covid pandemic.
In my opinion, as we live in a more polluted environment, taking prebiotic fiber and probiotics should be a part of everyone’s diet every day".
What is the best diet to help support lung health?
In my opinion the Mediterranean diet rich in fruits and vegetables, nuts and seeds, chicken and fish, and a small amount of meat is the best way to reduce inflammation.(10) Traditional Chinese Medicine recommends garlic, sweet potato, ginger, onion, cabbage, pears, walnuts, black pepper, radish, rice, chili, leek, cardamom, miso, broccoli, cucumber, celery, and bananas to improve Lung Energy/Lung Qi.
Prebiotic fiber intake improves lung function.
Dietary fiber should be part of our diet every day. A diverse gut microbiome benefits all aspects of our health, including the lungs. I recommend Baobab fruit powder for weight management and healthy blood sugar. Baobab fruit powder improves gut health and contains anti-inflammatory polyphenols and immune-enhancing vitamin C.
Omega 3 Fatty Acids reduce lung inflammation.
Adding Omega-3 fatty acids reduces inflammation and helps prevent and improve asthma and allergic diseases. Omega-3 oils are considered to have a prebiotic effect in the gut, increasing beneficial microbiota and the production of anti-inflammatory short-chain fatty acids. Actually. I would recommend incorporating fatty fish or algae in your diet wich are rich in Omega-3 fatty acids.
Daily lung support protects you from pollution and infection.
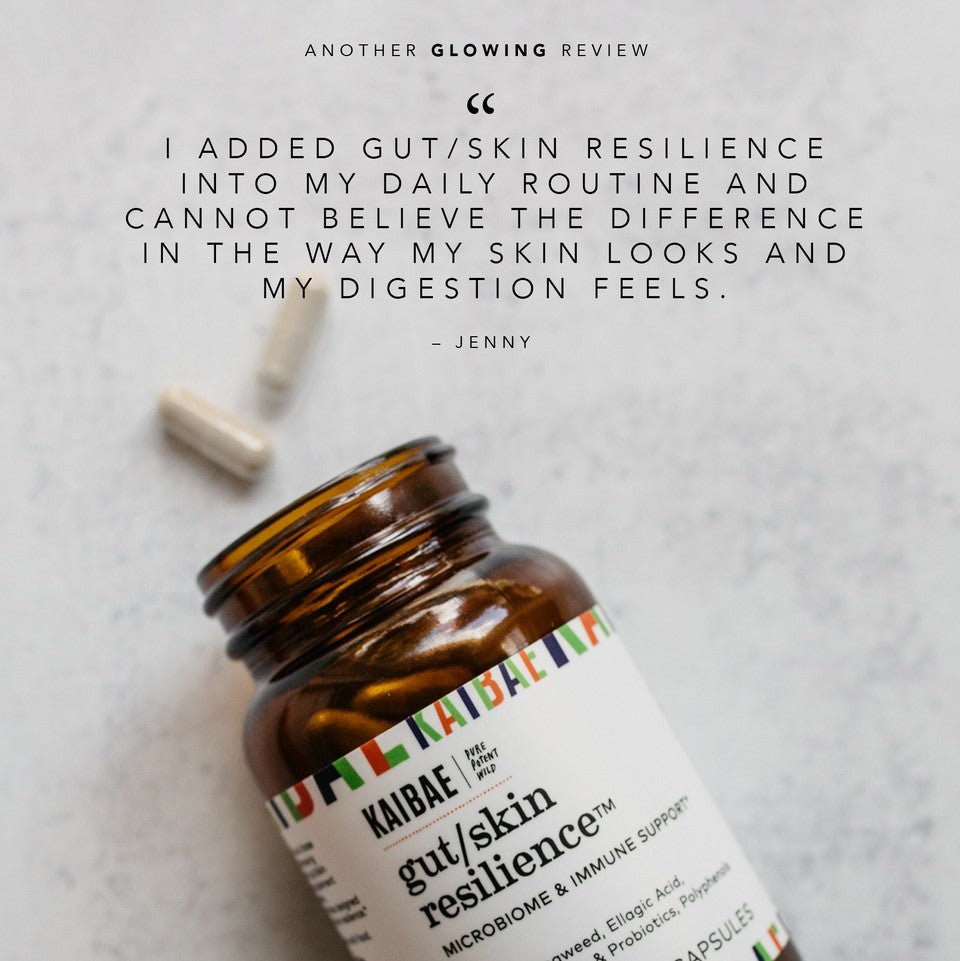
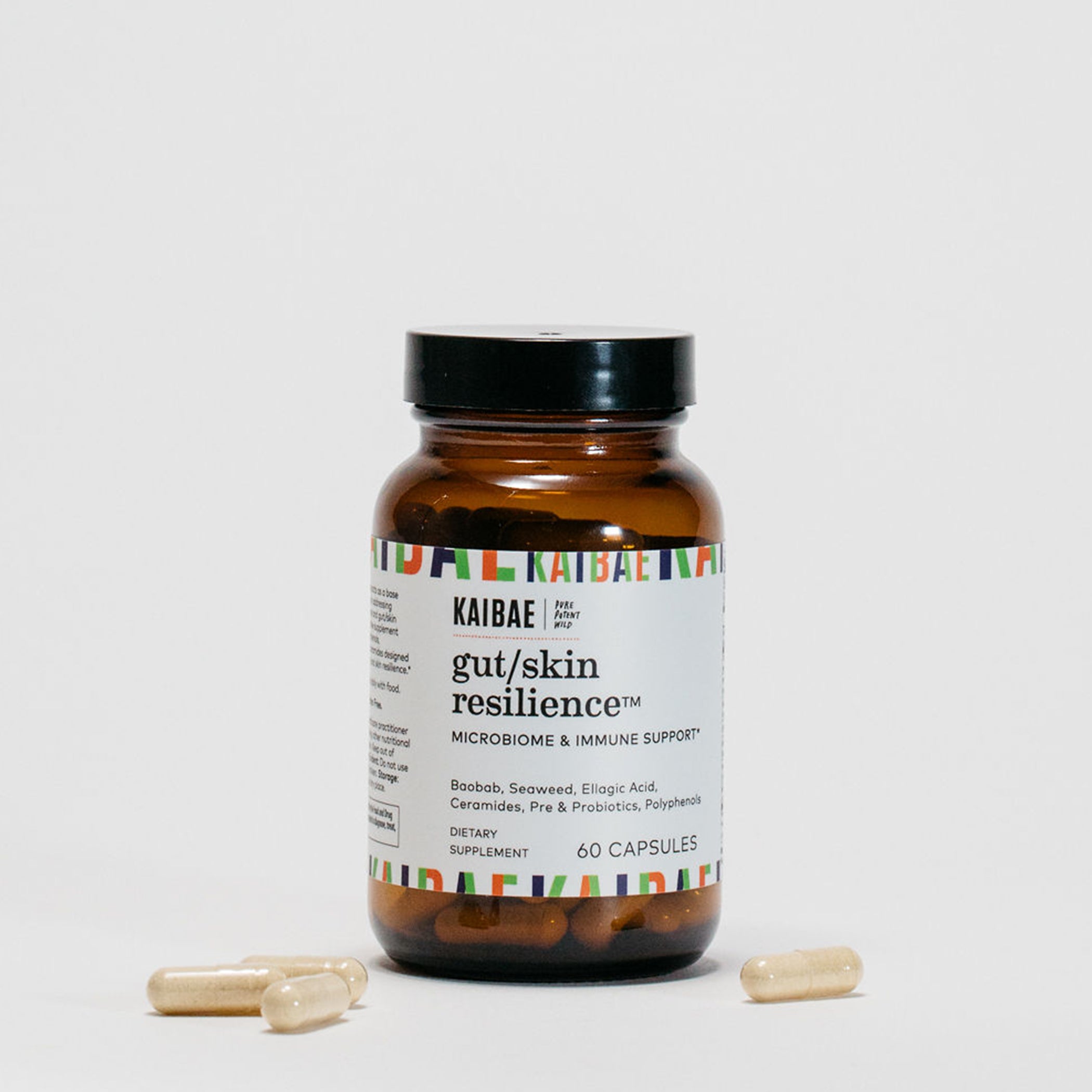
Gut/Lung Resilience is a lung supplement by KAIBAE that provides essential nutrients for a balanced gut-lung axis. A synergistic blend of prebiotic, probiotic, and wild plant polyphenols helps defend against infection and the effects of pollution.
Gut /Lung Resilience is a supplement to always have in your medicine cabinet and a travel companion to keep you healthy while on the go!
- Pelargonium: Wild-harvested mucolytic & antiviral support
- Baobab: High in vitamin C, polyphenols & prebiotic fiber to boost immunity
- Elderberry: Rich in polyphenols, great for lung & immune health.
- Beta-glucan; Immune enhancing prebiotic
- Lactospore: A probiotic that reconditions the gut, acts as an antioxidant and supports a healthy gut environment.
Improve your stress response for healthier lungs
KAIBAE's Stress Resilience, is a mood support supplement that promotes a healthy stress response through the gut-cortisol-brain axis. A synergistic blend of prebiotic, probiotic, and wild polyphenols.
- Sceletium: Wild harvested polyphenol-rich plant helps moderate feelings of stress and anxiety.
- Baobab: High in vitamin C, polyphenols & prebiotic fiber to boost immunity
- Ashwagandha: Helps endurance, memory, and cognition.
- Magnolia bark: Elevates mood and relieves pain
- Lactospore: Spore biotic probiotic reconditions the gut, acts as an antioxidant and supports a healthy gut environment.
Breathing exercises improve lung function.
I recommend the Book BREATH by James Nestor. Conscious breathing has excellent health benefits, from strengthening the lungs to promoting weight loss, improving increasing energy, and calming the mind.
Physical exercises improve lung function.
Physical exercise strengthens your lungs, increases lung capacity, and helps clean your lungs. Exercise also increases muscle mass and reduces insulin resistance, contributing to lung dysfunction.
Conclusion
Building resilient lungs may very well be one of the most important things we can do for our health, especially now as we navigate this time of Covid, a virus that stresses our lung health, sometimes creating permanent lung damage.
For those living in urban environments, external factors such as increased exposure to toxins and allergens make us more susceptible to bacterial and viral infections. While wearing masks in crowded and polluted environments and adding filters to our homes and workspaces is extremely important – the key to fully supporting your respiratory health greatly depends on what we do from within!
Whether you live in an urban, suburban, or rural setting, the choices you make around food, exercise, stress management, all play critical roles in the health of your respiratory system. Focusing on lung health is now more critical than ever as we all navigate the era of Covid and an increasingly polluted environment.
Starting with gut health is something everyone can do. Making dietary choices rich in anti-inflammatory foods, refining your nutrient intake with prebiotic-rich Baobab Superfood Powder and Baobab Wellness Tea, and supporting the lungs from within with Gut/Lung Resilience by KAIBAE are great ways to start building healthy, resilient lungs.